The 8-minute rule allows doctors and practitioners to bill Medicare for one service if the length of service is at least eight (8) minutes. But on the other side, the service must be under 22 minutes to be considered as one unit. In this blog, we will break down what the 8-minute rule is, how the 8-minute rule works in the case of physical therapy, and to what parts of Medicare it applies.
What is Medicare’s 8 minute Rule?
The 8-minute Rule applies only to Medicare Part B. It is created for outpatient services, specifically skilled services like physical therapy. The rule permits medical personnel to bill for units of service given, under one condition – length of time. Service must be given for at least eight minutes, and no longer than 22 minutes to be considered as one billing unit. Units of service consist of 15-minute intervals.
The 8-minute rule allows medical personnel, most usually rehabilitation therapists, to precisely determine the number of units they can bill for specific services and the length of time service is given. The 8-minute rule generally applies to Medicare billing, but it is not limited to it, because some private outpatient providers may also use it as well. But in this blog, we will be focused only on the Medicare billing unit 8-minute rule.
The 8-minute rule only applies to certain services – specifically skilled services that are billed with time-based codes. There are a couple of different qualifications for skilled service, but the key one is that the services, observations, or treatment plans require the involvement of medical personnel to meet the patient`s needs. For example, skilled services are therapeutic exercises or activities that require the supervision of a qualified provider, as well as a range of motion exercise and the services of an SLP when necessary for the restoration of function in speech or hearing.
In addition to the stated requirement, the 8-minute rule is also only required for any time-based services.
Medicare 8 minute Rule Billing Guidelines
The given service must be provided for at least eight minutes to obtain reimbursements of costs. You must receive at least eight minutes of treatment time to enter the 8-minute rule and be covered for another 15 minutes of service.
Let`s see how it works in a real-life situation. If the given service is 17 minutes long then Medicare will be billed for a single unit (15 minutes). On the other side, if the given service is 23 minutes long then Medicare will be billed for 2 units because after 15 minutes treatment continued for 8 more minutes and you enter in the second unit of service. The invoice would still be for two units regardless of whether you spent 23 or 30 minutes using a certain service.
Be aware that this rule only applies to one-on-one services with direct contact, with therapists working exclusively with one patient for at least 8 minutes. If the given service was provided for less than 8 minutes, Medicare won`t be billed for it.

Medicare 8 minutes Rule Chart
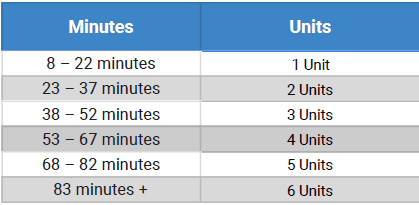
An 8-minute rule chart is a specific tool that helps understand and determine how many units should be provided and how to bill it properly.
The formula for counting costs is the following: first, add up the total number of minutes provided in therapy. Then divide the given result by 15 to get the number of units. If the leftover is 8+ minutes, the provider can bill for one more unit. If the leftover is less than 8 minutes, it is not possible to bill for any extra units. If the care is provided for 16 minutes, the provider can only bill for one unit.
Timelines in the code book for service units are sorted this way:
The 8 minute Rule in Physical Therapy
Time interval is the main factor for coding physical therapy codes. As introduced, Medicare has a special 8-minute rule for physical therapy procedures. But first, we need to learn about CPT codes and what they are.
Medicare’s 8-Minute Rule for time-based codes is invented for physical therapists for proper billing of physical therapy codes. Some CPT codes are based on the time used for the exam – time-based CPT codes. For example, in moderate sedation, there are separate codes for the initial 15 minutes of service, and for additional 15 minutes, there is another CPT code meant to use. In the same way, there are physical therapy codes based on time.
Below are the physical therapy medical codes used by the medical coder:
97001 Physical Therapy Evaluation
97002 Physical Therapy Re-Evaluation
97110 Therapeutic exercises
97140 Manual Therapy
97530 Therapeutic Activities: Use of dynamic activities to improve functional performance
97112 Neuromuscular Re-education
97113 Aquatic therapy
97116 Gait training
97124 Massage
97014 Electrical stimulation
97012 Traction, mechanical
97010 Hot or cold packs
97033 Iontophoresis
97035 Ultrasound
97034 Contrast bath
97036 Hubbard tank
97139 Unlisted procedure
97039 Unlisted modality
So, now let`s see how it works in real physical therapy services examples. The patient is given therapeutic exercise (code:97110) for 35 minutes, and after that is provided with manual therapy (code: 97140) in length of 15 minutes. Here the total time spent is 50 minutes (35 + 15). Divide 50 by 15 for a result of 3.3, leaving 5 remaining minutes. For this service, the billable unit is 3 units since the leftover minutes equals 5, which is less than the required 8 minutes. If there was a residue of 8+ minutes, then the therapist could bill for an additional unit, and then in total, it would be 4 units.
Medicare 8 minute Rule Common Questions
Does the 8 minute Rule Apply to Medicare Part A?
It does not apply to Medicare Part A, because Part A is inpatient coverage and it covers all the necessary services while you are admitted to the hospital. The 8-minute rule only applies to Medicare Part B, because it is outpatient coverage for outpatient services, which is suitable for all the rules applied on this matter.
The 8-minute rule in Medicare allows medical practitioners to charge Medicare for service per unit given. One unit last in a time interval of at least 8 minutes, and no longer than 22 minutes. The rule applies to outpatient services covered by Medicare Part B.
How to Explain Medicare 8 minute rule?
Medicare 8-minute rule is specifically created for skilled services like physical therapy services. It applies to certain services provided by Medicare Part B that are marked with time-based codes. It is billed by units that show time spent on the service provided. One unit lasts for at least 8 minutes and no longer than 22 minutes. It is designed for medical personnel to precisely bill the given service.
Can a Physical Therapist Bill For Massage?
A physical therapist can bill for a massage if it is considered a therapeutic massage. Therapeutic massage includes kneading, plucking, wringing, hacking, skin rolling, cupping, and rhythmic percussion. It is marked under CPT code 97124 – massage therapy.
For more information read our blog about the 8-minute rule for physical therapy.
How Many Therapy Units are 40 minutes?
A billing chart formula for counting units is next: total minutes spent on therapy divided by 15 gives the number of units. In this scenario, 40 minutes divided by 15 gives 2,67 units. The result is rounded up to a larger number. So 40 minutes of therapy is 3 billable units.
Can a Physical Therapist Bill For a Documentation Time?
Billable time is time spent treating a patient. So, initial evaluation – assessment and management time, together with time spent on documentation is part of the billing process. However, if the only provided service is documentation then the therapist cannot bill that time.
What Does PDPM Mean For Therapists?
PDPM means Patient-Driven Payment Model. It is a new Medicare payment rule designed specifically for skilled nursing facilities. With PDPM, therapy minutes are removed as the basis for payment in favor of resident classifications and anticipated resource needs during the course of a patient’s stay.
How Group Therapy is Billed?
Group therapy is simultaneous treatment provided to a minimum of two patients who may or may not be doing the same therapeutic activity. If the therapist is in constant attendance, but not gives one-on-one contact, but divides attention between every patient, then it is appropriate to bill each patient for one unit of group therapy. Group Therapy is under CPT code 97150. This situation is known as mixed remainder.
How Many Minutes are 2 Units?
Two billing units are considered when the time spent on provided service is between 23 and 37 minutes.
What is a Billable unit?
A billable unit marks the time duration of service provided. One time-based unit of service consists of 15 minutes. The first unit starts after 8 minutes spent with a patient and lasts no longer than 22 minutes. From 22-37 minutes is considered as 2 units, 38-52 minutes are 3 units, 53-67 minutes are 4 units, etc.
Is 97110 a Timed Code?
The 97110 is a CPT code that marks foundational occupational therapy exercises that are designed to improve strength, range of motion, endurance, and flexibility. In order to bill the 97110 code it must be described as medically necessary for a patient. Also, the session must be active one-on-one work with the patient. So, the 97110 is a time-based CPT code with each unit duration of 15 minutes.
How is the Time Billed for Two Units?
Two units of time are considered when treatment time was 23-37 minutes long.
What Insurances Implement the 8-minute Rule?
The 8-minute rule is specifically designed for services under Medicare Part B. However, insurance companies with Medicare Assignment and those who follow Medicare billing guidelines may apply the 8-minute rule. Regarding that, Medicaid, TriCare, and CHAMPUS can use this special rule.

